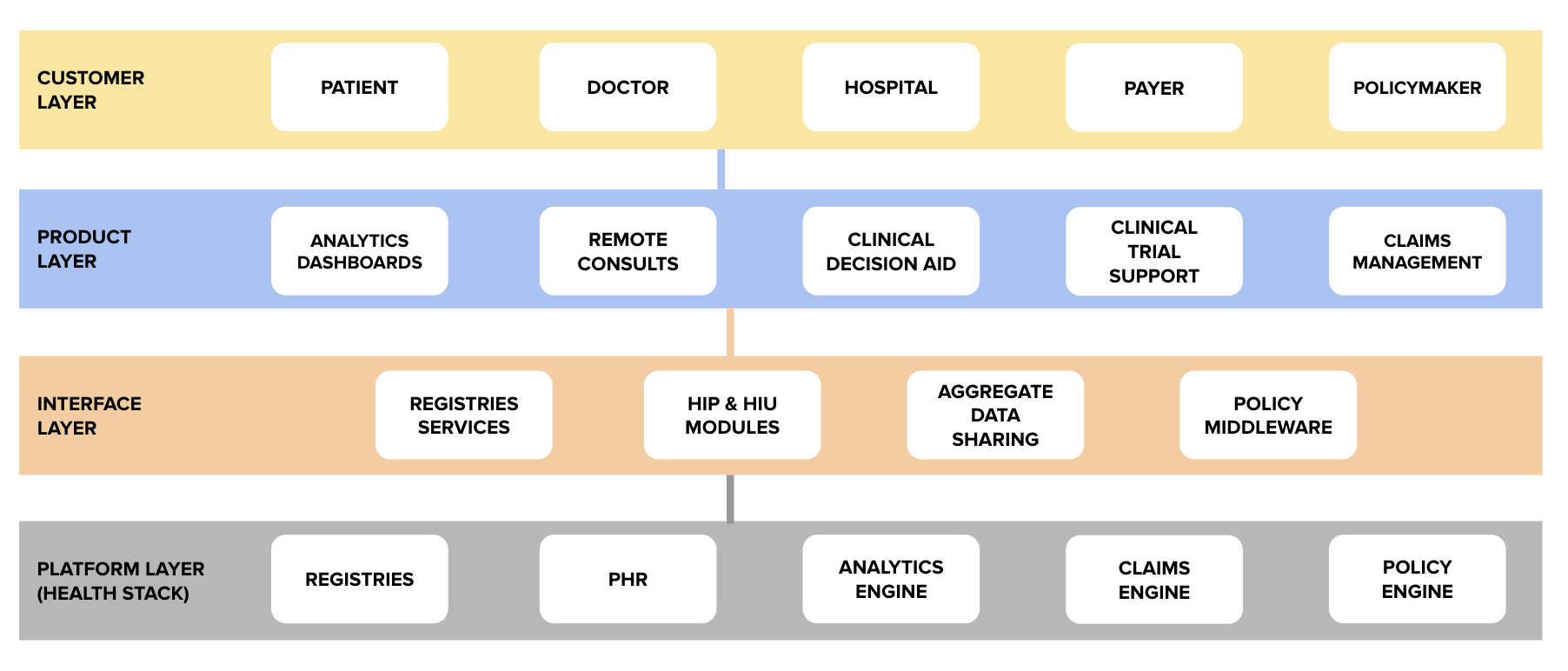
On 6th June, we marked the third open house discussion of the National Health Stack (NHS). At the beginning of the session, iSPIRT volunteer Sharad Sharma offered a brief recap of the NHS and painted a roadmap for future developments in this initiative (including timelines, agendas, and future open house sessions). Sharad also discussed the content of the most recent open house session, in which Kiran Anandampillai explained the concept of the electronic registry system. After reiterating the vision for the NHS and the registry system, Sharad passed the floor to iSPIRT volunteer Vikram Srinivasan to dive into the registry APIs.
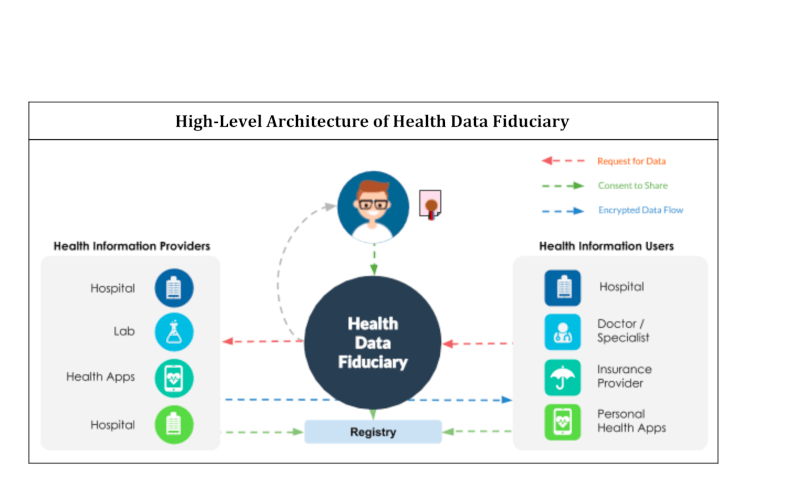
As a refresher, the electronic registry system is a mechanism for managing master data about different entities in the healthcare ecosystem. In today’ session, Vikram focused on the doctor registry. As the name suggests, the doctor registry will contain information about the doctors licensed to practice in India.
The doctor registry has the following design principles:
- Self maintainability: Doctors should be able to enrol themselves and update their own data
- Non-repudiable: The data in the registry should be digitally signed by a relevant attester (such as a State Medical Council) so that it can independently be verified by anybody
- Layered access: There should be a clear demarcation between public and private data in the registry, with only consent-based access to private data (eg. a doctor’s name and registration status should be public, but mobile number and photo should be private)
- Extensible schema: The data in the public registries should be as minimal as possible, allowing private players to build their own extensions around the core schema
- Open APIs: The data in the registries should be available via open APIs
- Incentive aligned: The registry must enable convenient use cases so that doctors have an incentive to keep it up to date (eg. doctors can use their registry profile to electronically sign prescriptions, insurance claims etc. or doctors can use their registry profile to streamline and digitize the process of renewing their medical licenses)
After discussing the design principles behind the registry, Vikram dived straight into the details of the doctor registry APIs, which can be broken into the following categories:
- Enrollment APIs: These APIs allow doctors to enrol in the registry and update their data
- Consented APIs: These APIs allow a doctor to authenticate themselves, share their data/profile, and electronically sign documents
- Search APIs: These APIs are used to access the registry to query a doctor’s public data or search for any other publicly available information
After covering these topics at a high level, Vikram released the API specifications for the Consented APIs and the Search APIs. The Swagger documentation for the same can be found here. The enrollment APIs will be released during next week’s open house session.
Upon completing his walkthrough of the doctor registry APIs, Vikram handed the floor over to our volunteer Siddharth Shetty. In the beginning of his segment, Siddharth answered the community’s technical questions around the NHS. Here are the questions he answered:
- Is it mandatory to use the Open Source Project Eka codebase that has been published for the Consent Manager, API Bridge, and Gateway?
- In case of the Schema Standardization, during the 1st schema-less phase, are HIPs allowed to share data formats like JPEG, PDFs etc?
- Can the consent manager give the health locker (as an HIU) a standing consent to keep pulling the user’s information from various HIPs on an ongoing basis i.e. bypass the consent manager for future requests
- Can the API bridges be configured such that instead of just sending the links to the information based on a request from an HIU (health locker in this case), the information can be sent such that it can be copied into the health locker?
- Will the consent artifacts be encrypted between parties using any asymmetric key mechanism which will be valid between the services?
- Is there any defined/recommended timeout for the data transmission from HIU – Bridge – CM- HIP and then HIU – HIP?
These were all great questions, and hopefully Siddharth’s answers helped clarify any doubts. If anybody wishes to ask any other questions around the NHS, please send them in to [email protected] with the subject line “NHS Questions”. Siddharth will continue answering the community’s technical questions during next week’s session (business-related questions will be answered in subsequent sessions).
To close off the open house discussion, Siddharth laid out the different working groups in the NHS ecosystem. Since the NHS is an open, public ecosystem, it is crucial for industry players and interested citizens to contribute to its development and pitch in with their feedback, knowledge, and engagement. Here are the working groups that are currently being formed:
- Technical Architecture Group: Responsible for working on open technical problems such as circuit breaker flows and time-out mechanisms. Also responsible for extensions and changes to the tech architecture
- Data Dictionary Group: This working group deals with moving away from the current schema-less architecture towards a standardized data vocabulary (leveraging existing medical schema projects and also coming up with new ideas relevant to the Indian context)
- Pilot Group: This group is comprised of people who have already started building on the NHS components (or would like to start building on the components).
- Ecosystem Incentives Group: This group is looking at the incentive structures that power the NHS ecosystem (monetary and otherwise)
Any readers who are interested in learning more or joining these working groups are invited to reach out to [email protected]. A complete recording of the 6th June’s open house discussion can be found below
During next week’s session, we will be covering the Personal Health Records system (PHR), particularly as it relates to hospitals, and we will also be diving deeper into the Doctor Registry Enrollment APIs.
Readers are advised that next week’s NHS open house discussion will take place from 11:30 am – 12:30 pm on Saturday, June 13th.
The registration form for next week’s session can be found here.