When was the last time you skipped a movie for a workout, or chose a salad over a pizza? Or, actually got your annual tests done – annually? Or, visited a doctor without seeking a second opinion? Or, took your pills without constant reminders?
These are problems even for someone who can afford the time and access to read blogs online. Now let’s move on to Bharat (i.e., all Indians except the affluent ~30 million families).
Remember the Gorakhpur hospital deaths last year? Or, the recent Bihar encephalitis crisis? Here are some more boring stats – more than half the doctors in the country practise without any medical qualification, less than 20% of our population has access to secondary and tertiary care, more than 7% get pushed into poverty because of expenditure on healthcare every year. Be it tuberculosis, diabetes, anaemia or cancer – India shares one of the highest, if not the leading, burden of disease globally.
So, where is the problem? It’s everywhere!
Let’s step back a little. There are constraints, and then there are problems. Problems are those that can and should be addressed. Constraints, however, are things that are almost impossible to change. For example, there just aren’t enough qualified doctors in the country. Or, a single-payer and provider system (i.e., our public health system) simply cannot address all the healthcare needs of the country. It is impossible to create a large pool of doctors in a short amount of time. Similarly, we are bound to have multiple payers and providers, each of whom has fundamentally misaligned incentives. These constraints are inherent in the system.
The question is – can problems be solved while operating under these constraints?
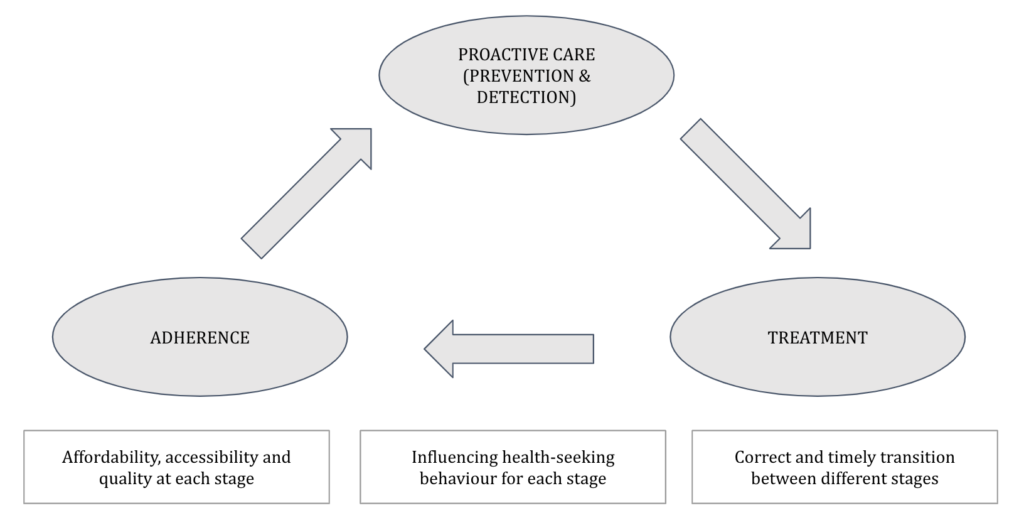
If we were to look at the problems, they would broadly be classified as the following:
- Supply (quality, affordability and accessibility): Improving quality, affordability and accessibility is indeed a necessary first step. While it is important to strengthen the existing infrastructure, certain initiatives and technologies can help accelerate this process. For example, the Ayushman Bharat Yojana is already addressing affordability at secondary and tertiary care levels for the vast majority of the population. Similarly, the combined use of low-cost screening and diagnostic devices, telemedicine and clinical decision support systems can enable even minimally trained professionals to deliver care, especially at the primary care level – making it good, affordable and accessible.
- Demand (health-seeking behaviour for preventive care and adherence): Even an excellent care delivery system would fail if people didn’t avail the services or didn’t stick to the recommendations offered as part of these services. This is precisely the problem in healthcare. Very few people actually engage in preventive care or adhere to the recommendations or treatment plan prescribed by a caregiver. It would require a very savvy use of point-of-care devices (that enable convenient at-home/doorstep testing, monitoring and instant diagnosis at affordable prices) and behavioural economics hacks (nudges) to bring about this behavioural change.
- Misaligned incentives (between provider-provider and payer-provider): An eye-care provider that I spoke to explained this to me. Even though this provider focused on cataract surgeries, it often ended up carrying out screening camps and post-op follow-up care for its patients. This was because of a lack of referrals – even if small providers/ general practitioners detected disease in the patient, they would not refer the patient upward for fear of losing to another provider. In other words, upward referrals don’t happen because downward referrals don’t happen. Similarly, the fundamentally misaligned incentives between payer and provider (which we talked about at length in this post) result in issues like procedure inflation and delayed intervention. How can this be addressed?
What’s missing?
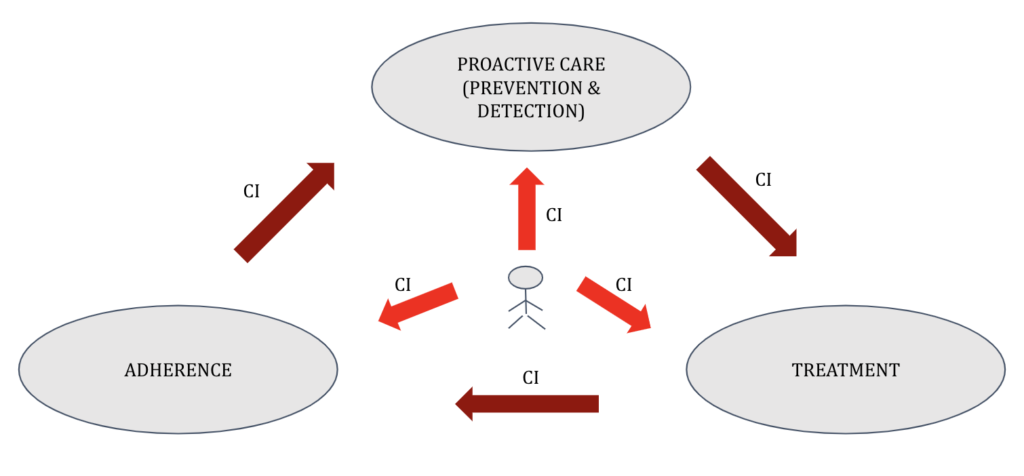
As mentioned in one of our previous posts, we think the answer might lie in the concept of care intermediaries. As the name suggests, these will be new types of independent entities that are different from payers and providers. They will act as agents of the patient and aid in decision making. Specifically, they will play the following roles: (a) aggregation, (b) nudges, (c) referrals, (d) audits. With care intermediaries in the picture, let us understand what the new normal would be:
- The care intermediary predicts preventive care-seeking behaviour, disease incidence and adherence patterns. It uses this intelligence to distribute appropriate gamifier policies to customers. As an aggregate buyer of these policies, it is able to provide them at reasonable costs to the end consumers while also providing for its own sustenance.
- Every person who has a gamifier policy is now nudged by the care intermediary to seek preventive care. The care intermediary also carries out appropriate screening and diagnostic tests for its consumers.
- For the consumers identified with a need, the care intermediary then becomes a part of the referral workflow, and makes recommendations to the patient for both procedure and provider selection.
- Lastly, the care intermediary facilitates downward referrals and nudges the patients to adhere to the prescribed post-treatment care plans.
There could be many manifestations of the care intermediary – for example, it may partner with local community health workers to carry out screening and adherence management. Or, it could partner with primary caregivers for providing the actual referral recommendation to a patient. In other cases, such as seeking a major tertiary care treatment like surgery, the patient may directly consult the CI for recommendations.
What’s next?
What will the business model of a care intermediary be? How will it make credible recommendations? Who will it partner with? What are the checks and balances required? What is needed from a privacy perspective?
The idea of a care intermediary is new, and a lot still needs to be worked out!
If you would like to share feedback or volunteer with us to help with this effort, please reach out to me at [email protected].