In the last few months, I have had the opportunity to work closely with the National Cancer Grid – a network of 150+ cancer centres in India – and in the process, better understand the workflows involved in different medical processes and the requirements of medical professionals. I have closely observed care delivery, interviewed cancer patients and oncologists, learnt about current challenges and about initiatives being undertaken by NCG and other organisations to tackle them.
This blog post is an evolved version of an earlier post, where I had talked about the use cases of health data and the implementation of a PHR (Personal Health Record). Of these, I believe that the biggest use of health data will be in improving the quality of care in complex medical cases (either acute like surgical procedures, or chronic like cancer). In this post, I will use cancer care to exemplify this.
Core idea
Let us visualise a specific application for cancer care, with oncologists as its primary users. There are only around 1000 trained oncologists in India, so let’s assume that all of them are users of this application. Let us also assume that clinical data of all patients treated by these oncologists is conveniently accessible through this application (with due privacy and security measures). What will these users do now?
Expert consultation
I attended a Virtual Tumour Board run by the National Cancer Grid – a weekly remote consultation program run on Saturday mornings where teams of doctors voluntarily join to discuss well-documented cases and their potential treatment plans. VTBs are run separately for each speciality (like head & neck tumour, gynaecology, neurology, etc.), which means that it takes up to 4-6 weeks for one’s turn. Doctors usually do not have the luxury of such long waiting periods, and therefore turn to individual consultations which are often not documented, depend on informal connects and are sometimes made with incomplete data. Formalising this process and making it asynchronous can be of huge benefit to all medical professionals.
Care team collaboration
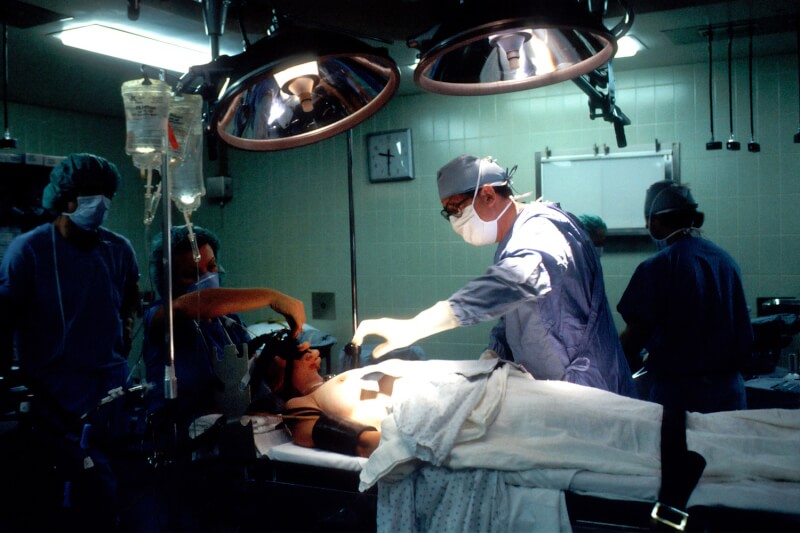
Complex medical procedures often involve a team of doctors and other medical professionals, working responsibly for a given patient. A significant percentage of all deaths due to medical negligence is caused by lack of communication between the care team members. The communication process today is paper-based and unstructured, leading to accidents that can, in fact, be prevented – especially with the growing use of IoT devices and voice-based inputs. (I saw one such application at Narayana Health being used by their ICU teams).
Performance evaluation
Lack of organised data, changing patient care-providers and long feedback loops make it difficult for medical professionals to monitor their performance. Can we empower them with tools to do so? Doctors today lack visibility on the outcome of the treatment given and rely on intuition, experience or techniques tested in developed countries for care delivery. Such a tool would not only help doctors improve their performance, but also improve the trust equation with their patients.
User Experience
There are three crucial elements for enabling a good user experience:
Data input – Most EHR systems require text input to be typed in by doctors. This makes it difficult to use. Other input techniques for automated data transcription like touch, voice, or other innovative methods for data capture will need to be explored. Additionally, interoperability across all systems and devices will be key in enabling access to all data.
Data interpretation – Sorting through a patient’s health records takes up a substantial amount of time of a physician, especially when the data is unstructured. Developing intelligence to sort the relevant records as per the case in question will significantly enhance the user experience of the product.
Safety and Privacy– All solutions should ensure complete privacy of patients. This could mean access controls, electronic consent, digital signatures, digital logs, tools for data anonymisation, etc. it might also be important to perform basic verification of users of the platform.
Value Discovery
The value of the platform will increase as more and more physicians become a part of it. For example, an endocrinologist might need to consult a cardiologist in a case of disease progression, or an ENT specialist might need to consult an oncologist to confirm a diagnosis. More importantly, the platform will also drive innovation, i.e., other use cases can be developed on top of it. For example, the expert opinions mentioned above can also be used for consulting patient remotely, pre-authorising claims, forming medical peer review groups, etc. Similarly, working care groups can also simultaneously enrol staff for upskilling (as practised today in an offline setting), and information about treatment outcomes can help guide better research.
Next steps
We remain on a quest to find use-cases for PHR since we believe technology pilots alone would not be enough to drive its adoption. In that context, we are looking for partners to experiment with this in different healthcare domains. If you are interested, please reach out to me at [email protected]!