Boost for HealthStack, but no gains for Industry
The Pandemic had decided much of the flow of financial planning in a country like India. The emphasis on Atma Nirbhar Bharat right at the outset in PART A of speech is on expected lines in a changed scenario post pandemic. Health being given importance forming the first pillar of six pillars was also expected based on ongoing developments.
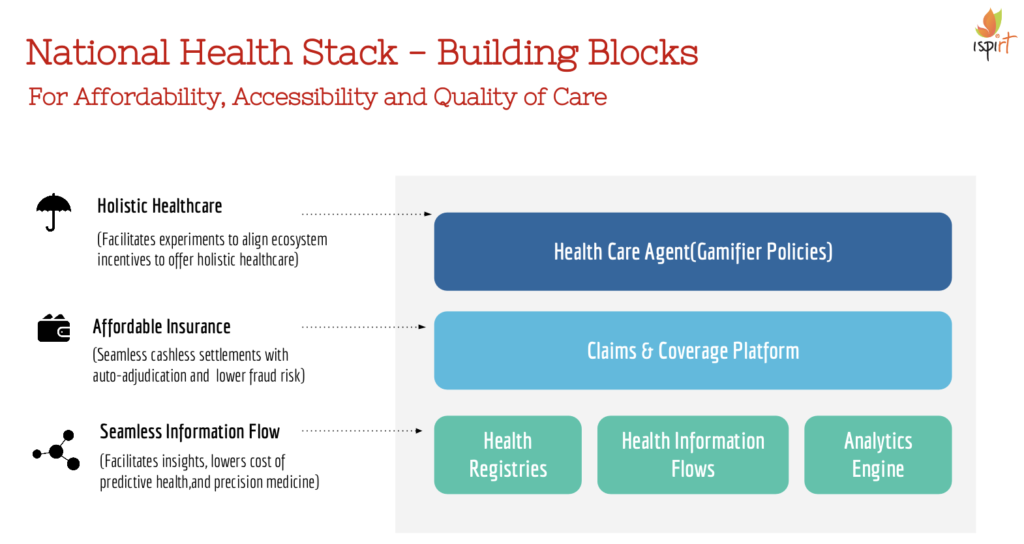
For decades, India has underinvested (both in public and private spend) in the overall health of the population, and it took a global pandemic to dedicate a new Pillar of the budget to improving health outcomes and increase funding by 130%. It is heartening to see a substantial budget allocation of 64,000 Crore towards the Aatmanirbhar Swasth Yojana to improve primary, secondary and tertiary care. With the National Health Authority getting veteran RS Sharma (former Chairperson of TRAI and UIDAI) as its new CEO, this scheme could be implemented in a digital-first manner taking advantage of the advanced architecture of the National Digital Health Mission.
At iSPIRT we are pleased to see this development, and look forward to a year of accelerated efforts to establish key public digital infrastructure that could improve healthcare.
It was also encouraging to see Innovation and R&D mentioned as one of the pillars; this is a sign the Government is keen on supporting an innovation driven economy and the Indian products eco-system. The National Research Foundation outlay of 50,000 crores over 5 years is applicable across all sectors. Production linked incentive (PLI) schemes were announced for 13 sectors. This is a welcome move to bring in a thinking of promoting Indian Product Champions. However, the details of structure and which sectors and playgrounds the Government is attempting to promote will determine the success in the global landscape.
At iSPIRT we have been advocating development of niche playgrounds in sectors where India has a competitive advantage such as Software products in all sectors including defense, telecom etc. Whether the outlay of 1.97 lakh crores, over 5 years starting FY 2021-22 will be enough is to be tested.
The Continued emphasis on digital payment promotion with a new proposal of 1,500 crores and not losing sight of startups movement is heartening for the Software product industry. Improving norms to formation of a 1 person company will encourage innovation, entrepreneurship and startups. The Government seems to also be inclined to use technology to improve compliance via faceless assessment and a reduced limit on reopening of assessment limits, which are also efforts in a positive direction.
The biggest missed opportunity was around support to MSMEs – which are the key to driving scalable innovation. The MSME sector continues to need life support post the pandemic. While the Government slotted in a 2X budget estimate for MSMEs, it is not clear what this will go towards or that it will help the sector at scale. What remains to be addressed is critical changes that could MSMEs, ease frictions to accelerate growth.
We wanted to see more action on Ease of doing business, especially around removing bottlenecks for tech companies across sectors. In a digital economy, the small business sector is the lifeblood of future growth, and the government will need to think hard about the true means of galvanising this sector.
About iSPIRT Foundation
We are a non-profit think tank that builds public goods for Indian product startup to thrive and grow. iSPIRT aims to do for Indian startups what DARPA or Stanford did in Silicon Valley.
iSPIRT builds four types of public goods – technology building blocks (aka India stack), startup-friendly policies, market access programs like M&A Connect and Playbooks that codify scarce tacit knowledge for product entrepreneurs of India. visit www.ispirt.in
For further queries, reach out to Sudhir Singh, email: [email protected] Or Karthik KS, email: [email protected]